You toss the quilt aside at 2 a.m. because your calves feel like they’re sprinkled with fire ants doing jazz hands.
Yesterday it was your scalp after a tough meeting, last week it was your ribcage right after you sprinted to catch a flight (thanks, TSA).
You’ve switched detergents, nixed wine, even bought the unscented everything—yet the itch keeps crash-landing on your skin like it got a VIP pass.
These stress hives don’t follow logic. They follow your nervous system.
What if the real mischief-maker isn’t the pollen, the pasta, or your “sensitive” skin?
What if it’s a nervous system stuck in high alert, churning out histamine like there’s a two-for-one sale on misery?
Mast Cell Activation Syndrome (MCAS) is the headliner, but behind the curtain sits chronic stress—rewiring your brain-skin hotline, stocking your dermis with extra mast cells, and flipping the itch switch at the worst possible moments.
This article is your roadmap through that maze.
We’ll dig into the science, decode the stress–histamine connection, and show you the next step toward turning down the static so your skin—and sanity—can finally breathe.
Key Takeaways
- Your skin and nervous system are biologically connected.
- Chronic stress increases mast cell activity and histamine levels.
- Healing starts with creating safety in the system.

Quick and Dirty: What Are Mast Cells and Why Are They So Sensitive?
Let’s talk about your body’s drama queens: mast cells.
These immune cells are like the neighborhood watch of your internal terrain (11, 17).
They live at the borders—your skin, sinuses, gut lining, lungs, and even your brain—keeping tabs on what’s coming in and what’s trying to sneak out (1, 8, 10, 11, 14, 17).
When they sense a threat (real or imaginary), they explode like over-caffeinated piñatas, dumping histamine, cytokines, prostaglandins, and other chemical “fireworks” into your tissues (1, 3, 8, 9, 10, 11, 12, 14, 15, 17).
Mast cells respond to neural, immune, hormonal, metabolic, and chemical triggers as well as pathogens (viruses, bacteria, parasites, etc.) (1, 8, 11, 14)
Think inflammation, itching, swelling, mucus, anxiety, even diarrhea (4, 9, 10, 12, 14, 15, 16).
Now, this system is genius when you need it—say, fighting off a parasite or healing a wound.
But in Mast Cell Activation Syndrome (MCAS), your mast cells have lost the plot. They’re triggered by non-threats like stress, heat, fragrance, or just… existing (1, 2, 4, 8, 9, 10, 11, 12, 14, 17).
It’s not just one reaction, either.
We’re talking flushing after a hot shower, hives from a hug, migraines after eating leftovers, or random panic attacks with zero emotional cause (4, 9, 10, 12, 15, 16).
That’s because mast cells don’t just release histamine—they influence your hormones, your nervous system, and even your mood (1, 4, 9, 11, 14, 15, 17).
In short: MCAS isn’t just a histamine issue.
It’s an immune regulation breakdown that turns your body’s best defenders into overzealous security guards, pepper-spraying everything in sight.
And the nervous system? It’s their boss.
And lately, it’s been yelling.
Histamine: Not Just About Hives and Runny Noses
If you’ve been told histamine is just that stuff behind your allergy symptoms—sneezing, hives, runny nose—you’ve only heard the G-rated version of the story.
The truth?
Histamine is more like a multitasking biochemical coordinator, moonlighting as a neurotransmitter, gut regulator, immune signaler, and, more.
Your body makes histamine on purpose.
It’s supposed to help you fight infections, digest food, regulate your hormones, and even stay awake.
But when histamine builds up faster than your body can break it down? That’s when the circus begins.
How We Can Help
Guiding people to reclaim their health and vitality is our greatest joy. Our entire practice is dedicated to supporting you to be who you really are, at home in your body, because your body is able to heal itself.
Book a CallLet’s break it down by source:
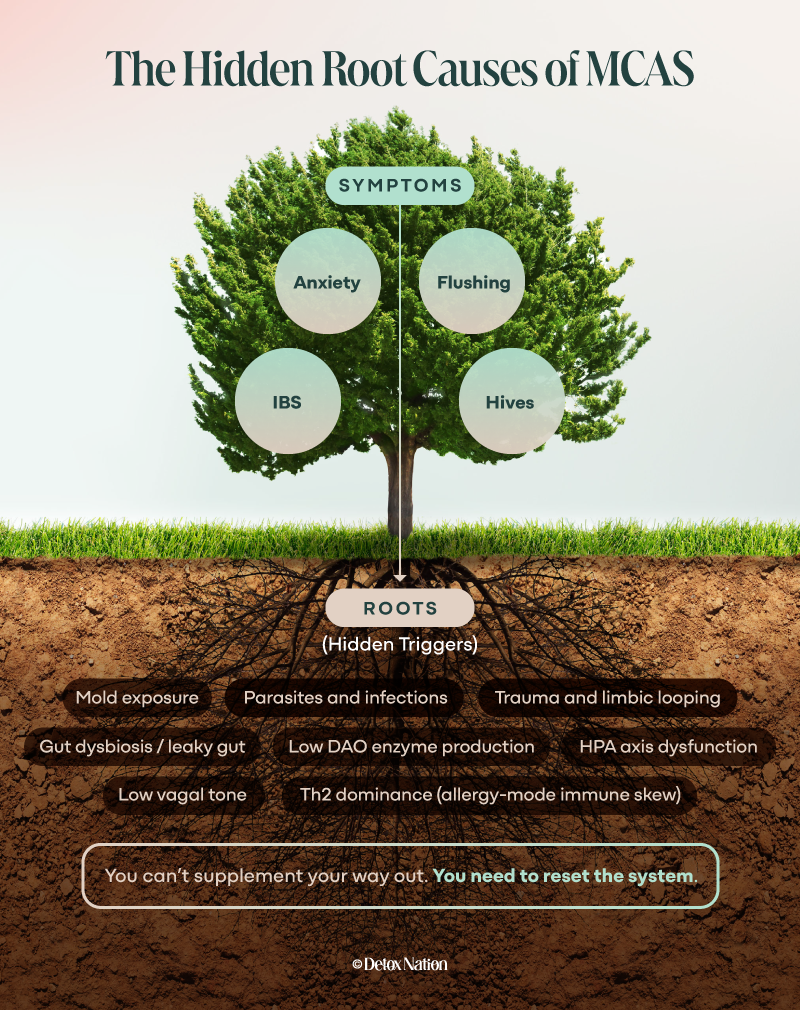
- Mast cells: The main producers of histamine when they degranulate (release their contents). In MCAS, they do this early, often, and with zero chill (1, 3, 8, 9, 10, 11, 12, 14, 15, 17).
- The gut: Certain bacteria produce histamine—and if your gut is leaky, inflamed, or missing beneficial strains, you’re likely absorbing more than you should (5, 16).
- Your food: Aged, fermented, processed, and leftover foods are naturally high in histamine. So are things like spinach, avocado, and yes—chocolate (don’t shoot the messenger).
- Your enzyme capacity: DAO (diamine oxidase) is your body’s main histamine-cleanup crew in the gut. But it’s easy to knock out—gluten, alcohol, gut infections, mold exposure, and nutrient deficiencies can all take it offline (5, 16).
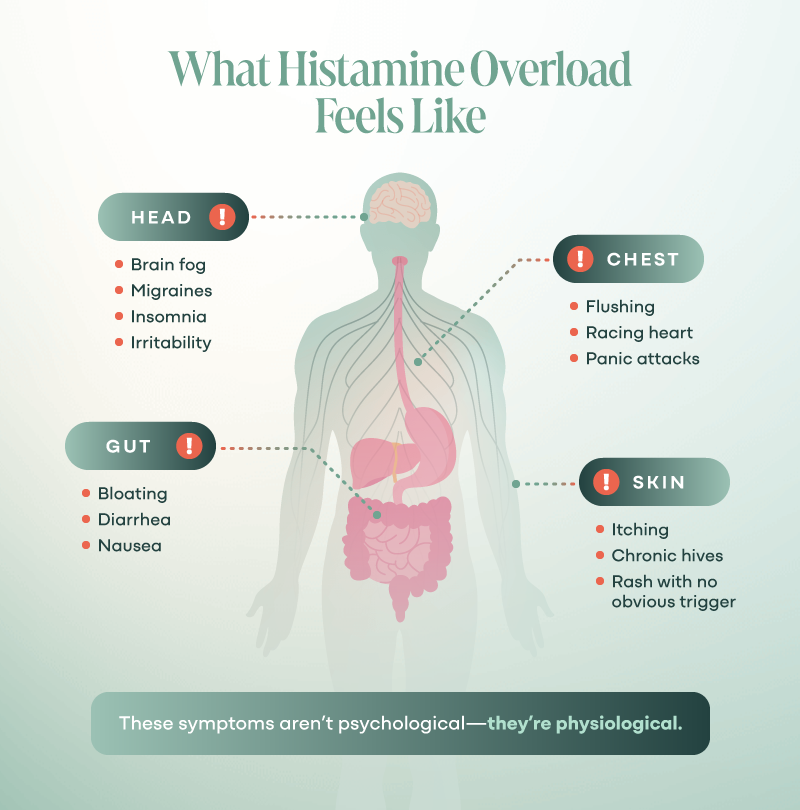
What does a histamine overload feel like (4, 9, 10, 12, 14, 15, 16)? Here’s a short list of greatest hits:
- Itchy skin with or without a rash
- Chronic hives
- Flushing after eating
- Insomnia that laughs in the face of melatonin
- Racing heart at rest
- Irritable bowels that play favorites with what they’ll tolerate
- Brain fog, headaches, anxiety—for no apparent reason
It’s not in your head. It’s in your histamine bucket—and it’s overflowing.
Your Nervous System and Skin Are Siblings
You might not have taken an embryology class (or maybe you skipped it—I wouldn’t blame you), but here’s a fun fact with massive implications for your health: your skin and your brain are literal siblings.
They both come from the ectoderm, one of the three primary layers that form in the earliest stages of embryonic development (13, 15).
Translation?
Your skin and nervous system were born from the same biological tissue.
So, it makes sense that they’re still in constant bi-directional conversation—like close siblings who never stopped sharing a room (13, 15).
This deep connection is why emotional stress shows up on your skin, why anxiety can cause hives or eczema flares, and why some people feel itchy just thinking about something stressful.

The brain-skin axis is a two-way communication channel—your thoughts and stress levels impact your skin, and your skin sends messages back up to your brain (13, 15). It’s a full-on feedback loop.
And when the nervous system is dysregulated—like when it’s stuck in fight-or-flight?
That communication gets glitchy.
The skin starts to behave like the body is under attack, because the nervous system is telling it so. Cue the mast cells. Cue the histamine. Cue the itch that won’t quit.
This isn’t psychosomatic. It’s neuro-immunological.
Stress: The Itch You Can’t Scratch
Chronic stress doesn’t just make you feel tense—it physically rewires your body’s operating systems (6). Especially your skin.
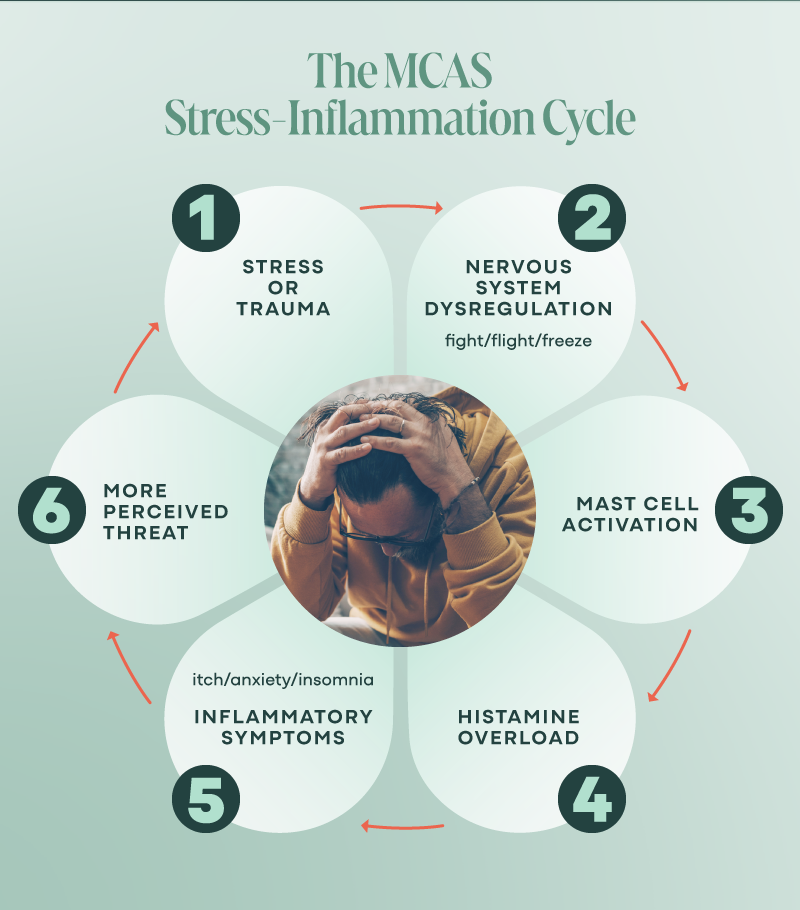
When you’re under constant stress, your nervous system can get stuck in sympathetic dominance—the “fight, flight, freeze, or fawn” mode that was designed for short-term survival, not long-term living.
In this state, your body reroutes energy toward defense, not digestion, detox, or repair.
And your immune system? It starts scanning for threats with a hair trigger. Mast cells get the memo first (15).
Research shows that stress increases both the number and sensitivity of mast cells in the skin and brain (17).
It also boosts the density of nerve fibers in your dermis—the layer where those mast cells hang out (15).
More nerves mean more “conversations” with mast cells, which means more histamine dumped into the skin in response to every little poke or prod (15, 17).
A stressful meeting, a poor night’s sleep, a tough workout, or even just a memory of trauma and suddenly you’re itching like you rolled in fiberglass.
The real kicker? The histamine and inflammation that get triggered by stress amplify the stress response (15, 17).
That means your nervous system can start interpreting your own biology—your own itch—as a threat.
It’s not just that stress makes you itchy. The itch itself becomes a stress signal. And that’s a vicious cycle worth breaking.
The Vagus Nerve: Your Body’s ‘Chill Out’ Switch
If your sympathetic nervous system is the gas pedal, the Vagus nerve is the brake—and in Mast Cell Activation Syndrome, your brakes might be shot.
This wandering nerve (Vagus = “wanderer” in Latin) runs from your brainstem down through your neck, heart, lungs, and digestive tract, acting as the command center for your parasympathetic system—aka rest, digest, detox, and heal (5).
It’s like your body’s internal therapist, whispering, “You’re safe. We can let go now.’
So, what happens when the Vagus nerve is sluggish, under-stimulated, or just plain ignored (18, 20)?
- Inflammation goes up.
- Histamine clearance goes down.
- Mast cells lose their chill.
- Digestion slows.
- Detox grinds to a halt.
- And yes—itching gets worse.
In my experience, low vagal tone is common in folks with trauma histories, mold illness, unresolved infections, chronic stress, or gut dysfunction (which, if you’re reading this, is probably you).
The good news? You can retrain your Vagus nerve (more on this later). Like any muscle, it gets stronger with use.
Supporting vagal tone isn’t just “nice to have”—it’s foundational if you want to stop living in reactivity.
Because when the Vagus nerve is online, mast cells stop overreacting. Your gut starts absorbing. Your brain stops panicking. And healing becomes physically possible again.
The HPA Axis: How Burnout Becomes Biology
You might feel like you’re just tired.
But your hypothalamus, pituitary, and adrenal glands—the HPA axis—know you’re running a full-blown emergency broadcast system. All. The. Time.
This trio coordinates your body’s response to stress, flooding your system with cortisol and adrenaline to help you “survive” the moment.
Trouble is, modern life is the moment—relentless deadlines, unresolved trauma, gut infections, EMFs, moldy homes, toxic bosses—and your body hasn’t caught on that the tiger is now an inbox.
Over time, chronic stress rewires the HPA axis (15), leading to:
- Cortisol resistance (your cells stop listening)
- Flattened cortisol rhythms (fatigue in the morning, wired at night)
- Poor communication between the brain and immune system
- Increased mast cell activity and permeability of the blood-brain barrier (17)
- More mast cells in the brain itself, especially the hypothalamus—the literal control tower of your HPA axis (3, 17)
This isn’t “adrenal fatigue” in the pop-wellness sense.
It’s your stress-response system throwing up its hands and saying, “We can’t keep up.”
And when the HPA axis is dysregulated, levels of inflammatory mediators like histamine rise (7).
Cortisol normally helps keep inflammation and mast cells in check—but if your body stops producing enough, or if your cells stop responding?
Mast cells start to party like the chaperones left the dance.
Even worse: this dysregulation commandeers your sleep, gut motility, hormone regulation, and brain function.
The HPA axis isn’t separate from your skin or immune system—it drives how they behave. And in MCAS, it’s often the silent ringleader behind the chaos.
Th2 Dominance: When Your Immune System Gets Stuck in Allergy Mode
Your immune system isn’t one big brute force army—it’s a balanced coalition.
When things are running smoothly, there’s a natural push and pull between Th1 and Th2 responses: Th1 handles viruses and cancer cells (the gritty hand-to-hand combat), while Th2 takes care of parasites, allergens, and wound repair (the cleanup crew with a tendency to over-decorate).
But chronic stress, toxin overload, unresolved infections, and gut dysfunction?
They tip the scales hard toward Th2 dominance (15). And that’s where mast cells really start acting out.
In Th2 dominance:
- Your body interprets benign substances as threats (pollen, food proteins, dust, your favorite blanket)
- Mast cells are over-recruited and hyperactive (15)
- Cytokines like IL-4 and IL-13 get upregulated, increasing IgE and histamine production
- You lose your tolerance to your own environment—and sometimes, to yourself
It’s like your immune system is stuck in “allergy mode,” launching over-the-top responses to mild stimuli.
And if you’re already dealing with mold, parasites, or viral reactivations (like Epstein-Barr or HHV-6), they’ll push this response even further.
That means more inflammation, more histamine, and more misfiring skin and gut symptoms.
And guess who drives Th2 dominance in a chronically stressed body? That’s right: our old frenemy, the HPA axis.
This is a logical (though miserable) adaptation to a body that feels under siege.
Thankfully, immune balance can be restored—but not by throwing random supplements at it.
You’ve got to create safety in the system first. Then the immune fog begins to clear.
Histamine, the Brain, and the Itch Loop
Let’s talk about the itch no one’s talking about—the one happening inside your head.
Yes, there are mast cells in your brain (15, 17).
That’s not a metaphor—it’s a documented fact.
They hang out in high-traffic areas like the hypothalamus, thalamus, and meninges (the lining around your brain and spinal cord).
These areas regulate sleep, temperature, mood, memory, and how your body perceives safety or threat.
Under normal conditions, they’re helpers.
But under chronic stress?
The number of mast cells in your brain increases (15, 17). And once they’re there, they don’t sit quietly.
Brain mast cells release histamine just like the ones in your skin.
But in your brain, that histamine doesn’t just make you itchy—it impacts neurotransmitters like dopamine, serotonin, and GABA.
It fuels anxiety, panic, irritability, and insomnia.
It keeps your limbic system hyper-alert, scanning for danger, convinced the world isn’t safe (even if you’re just trying to grocery shop without losing it in the produce aisle).
This is how histamine becomes a neuroinflammatory loop (15):
- Stress → more brain mast cells → more histamine
- Histamine → more anxiety, insomnia, sensory sensitivity
- Anxiety → more stress → more mast cells… and so on
And this is often why “mental health” interventions don’t work for folks with MCAS.
It’s not just psychological—it’s physiological.
Your brain’s histamine load is turning up the volume on your entire experience of life.
It’s also why even thinking about something stressful can trigger a flare.
Your brain doesn’t need a physical allergen to dump histamine—it just needs a reminder that you don’t feel safe.
Breaking this loop requires calming the brain from the inside out—not numbing it, not overriding it, but creating the right environment for it to stand down.

What You Can Do: Reset the Loop
By now, you’re probably wondering: “Okay, but how do I stop the madness?”
You can’t live in a sensory deprivation tank, and bubble-wrapping your life clearly isn’t working.
Here’s the empowering truth: you can’t eliminate all stress, but you can retrain how your body responds to it. And that’s the key to calming mast cells, reducing histamine, and breaking the itch loop—for real.
A body that feels safe doesn’t need to overreact.
Start Here: Nervous System First
You can’t detox from a fight-or-flight state. You can’t heal gut lining or balance hormones while your Vagus nerve is offline. Start by regulating, not pushing.
- Breathwork with longer exhales (5-7 seconds out)
- Cold splashes to the face or a cold pack on the chest
- Humming, tapping, or chanting
- Consider histamine-aware nervous system supplementation support like NeuroProtek Low Phenol
- Safe, slow somatic movement (like stretching, gentle yoga, craniosacral therapy)
- Daily dose of “earned safety” — time in nature, laughter, deep connection
Nourish Your Terrain
While you calm your nervous system, support your body’s ability to reduce histamine and inflammation:
- Low-histamine diet, short-term: helpful to empty the bucket while root causes are addressed (no fermented, aged, leftover foods for now)
- Support histamine breakdown with a balanced formula like Tessamet, and DAO enzyme production with vitamin C, B6, copper, and magnesium glycinate
- Rebuild gut lining with amino acids, bitters, and gentle binders
- Check for mold, parasites, or chronic infections—don’t guess, test
Work Strategically, Not Aggressively
- No “more is more” detoxing—overdoing it when your nervous system is dysregulated will backfire (detox can become a trauma trigger)
- Open drainage pathways before you mobilize toxins (Rapid Liver Reset is built for this)
- Think “flow over force”—your body will heal if you stop interrupting the signal
From Fire Ants to Flow
If you’re itchy, wired, inflamed, exhausted, and ready to scream the next time someone suggests “just try meditation,” I see you.
What’s happening isn’t random. Your body is brilliant—it’s responding to a nervous system that’s been stuck in survival mode for way too long.
That mast cell overreaction? That histamine overload? That skin crawling sensation at the worst possible moment?
It’s all part of a larger pattern: a body that doesn’t feel safe can’t heal.
But you can change the pattern.
Not overnight. Not by pushing harder. By creating the right internal conditions for safety, regulation, and flow.
That’s why we created tools to help you retrain your system—starting with the most important terrain of all: your brain.
Ready to Break the Loop?
Book a call with our team to learn which level of support is right for you. Let’s discover the root causes driving your symptoms, so you can resolve them for good.
Book a CallFAQs
Is histamine always bad?
No—histamine plays essential roles in digestion, immune defense, and brain function. It’s only a problem when your body can’t clear it fast enough or your mast cells won’t calm down.
Can stress really cause physical itching?
Yes. Chronic stress increases mast cell sensitivity and nerve density in the skin, making it more reactive—even without a visible rash.
What’s the connection between the nervous system and skin?
They both originate from the same embryonic tissue (ectoderm) and are in constant communication. When one’s dysregulated, the other reacts.
What’s the role of the Vagus nerve in MCAS?
The Vagus nerve helps regulate inflammation and mast cells. Low vagal tone can lead to more histamine, poor digestion, and a nervous system stuck in high alert.
Why does detox make me feel worse?
If your nervous system isn’t regulated and your drainage pathways aren’t open, detox can trigger mast cells and make symptoms worse.
Can I heal from MCAS?
Yes—but it takes a layered approach. Nervous system regulation, toxin removal, immune balance, and gut repair all matter. Healing is possible.