You wake up with that dull pressure behind your eyes, that swampy post-nasal drip, that weird ache in your upper teeth like your face is plotting against you.
If you’ve found yourself wondering, “Why do I keep getting sinus infections?”, you’re not alone.
Recurring sinus infections are a red flag that something deeper is out of alignment. Something real. Something your average ENT won’t test for, much less talk about.
You’re here because you’re ready to stop putting duct tape on the dam.
You want to know why this keeps happening, and more importantly, what to do about it. And that’s exactly what we’re going to unpack together.
So, take a breath. Get comfy. Let’s talk about what your sinuses have been trying to tell you.
Key Takeaways
- Chronic sinus infections are signals from your body that something is wrong.
- Many chronic sinus cases involve pathogens shielded by biofilms or fueled by hidden infections like mold colonization, parasite migration, and viral reactivation.
- This is fixable! You don’t need another round of antibiotics, you need a new strategy.
Recurrent Sinus Infections: A Signal
Having one sinus infection a year is annoying. Having multiple? That’s soul-sucking.
You start scheduling your life around when you’re probably going to get sick again.
You lose sleep (and your sense of smell).
You cancel plans.
And maybe worst of all, you start to wonder if this is just your new normal.
What you could be dealing with is a condition called chronic rhinosinusitis (CRS), which sounds fancy, but it just means your sinuses are inflamed most of the time, and mucus can’t drain properly (4, 12, 16).
This leads to a perfect storm: trapped pathogens, swelling, irritation, and pressure (10, 13, 14, 19). Over and over again.
But CRS isn’t a root cause. It tells you what is happening, not why.
Symptoms like (2, 5, 10, 14, 19):
- Constant congestion or facial pain
- Post-nasal drip that feels like glue
- Sinus headaches that laugh in the face of ibuprofen
- Endless fatigue, brain fog, and even dizziness are your body’s way of signaling something deeper is going on, something interfering with your immune system, your drainage, and your ability to heal.
Let’s get into what drives these flare-ups and why they keep coming back even when you’ve “done allll the things.”
The Sinus Ecosystem: What’s Supposed to Be Happening
Your sinuses are self-cleaning, unless something’s blocking the flow.
They are part of your body’s front-line defense system (12, 13, 14, 17).
Think of them like a well-tuned airport security system: filtering out invaders, scanning for threats, and keeping things moving so nothing gets stuck and causes a pile-up.
Here’s how that system should work:
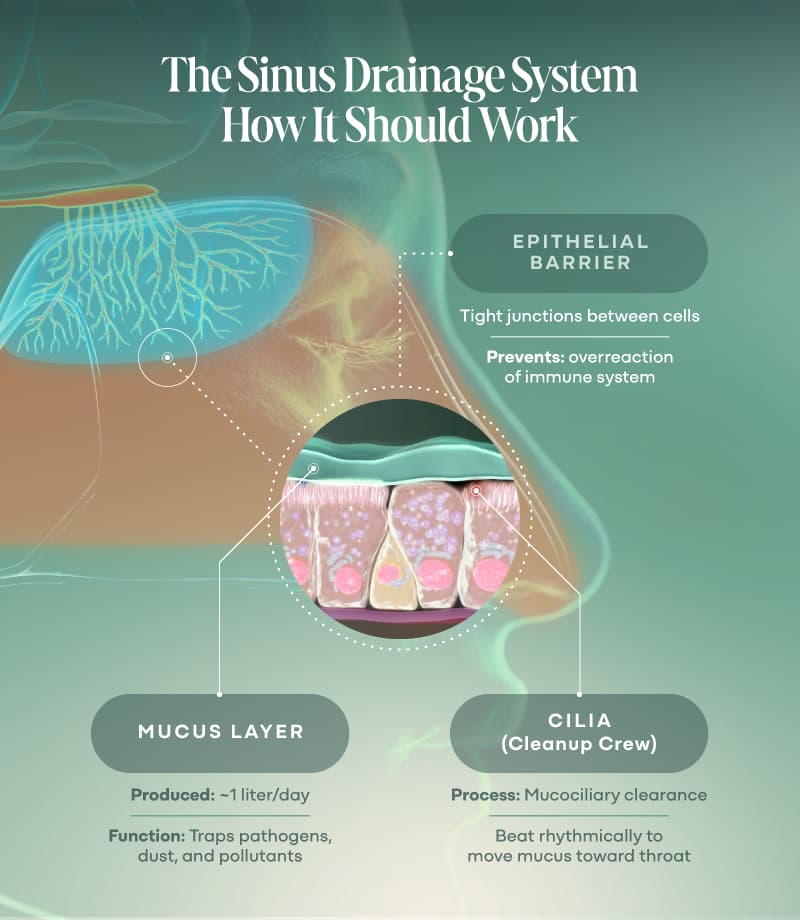
Mucus: Your First Line of Defense
Your body produces about a liter of mucus a day.
It traps dust, pollutants, microbes (even mold spores) and acts like flypaper for anything that doesn’t belong.
Cilia: The Cleanup Crew
Tiny hair-like structures called cilia line your sinus walls.
Their job is to move that mucus up and out toward your throat where it gets swallowed and neutralized by stomach acid (nature’s own bleach, basically).
This is called mucociliary clearance, and it’s a critical part of your innate immunity.
Epithelial Barrier: The Bouncer at the Door
The cells lining your sinuses form a tight barrier that keeps harmful substances out while allowing helpful ones (like nutrients and immune messengers) in.
When this lining is inflamed or damaged, that barrier gets leaky and suddenly your immune system is dealing with a constant stream of false alarms.
But when this flow gets blocked by swelling, thick mucus, infection, or even a shift in your internal terrain, that’s when things go sideways (10, 13, 14, 19):
- Mucus thickens and stagnates
- Cilia slow down or stop working altogether
- Pathogens stick around longer than they should
- Inflammation ramps up like a smoke alarm stuck in “test mode”
In other words: your sinuses stop draining and start stewing.
And when that cycle repeats enough times, you’re not just dealing with “a sinus infection.”
You’re stuck in a chronic inflammatory loop, and your body is doing its best to adapt under pressure.
Up next, we’ll break down the hidden root causes that sabotage this system from the inside out.

Hidden Root Causes That Sabotage Healing
If you’ve been treating chronic sinus issues like a series of random infections, it’s time for a reframe.
What if your body isn’t broken or weak, it’s just stuck fighting battles it was never designed to win alone?
That’s the case for most chronic sinus warriors I work with. Their immune systems aren’t lazy; they’re exhausted. Constantly responding to things they shouldn’t have to manage because the deeper terrain is off.
Mold: The Toxic Roommate You Didn’t Know You Had
Mold spores can colonize inside the body, including your sinuses (1).
There are also fungal fragments to consider. Just like the name implies, these are pieces of spores and mycotoxins produced by fungi.
One study found five hundred times more fungal fragments than spores (1). Additionally, the fungal fragments are deposited in respiratory tissues (including the sinuses) at a rate 230 times that of spore deposition (1)!
Certain molds like Aspergillus and Candida can produce their own biofilms and release mycotoxins, which inflame tissues, suppress immune function, and worsen drainage (1, 7, 13, 15, 17, 20).
And mold doesn’t usually travel alone; it often rolls in with MARCoNS (Multiple Antibiotic-Resistant Coagulase-Negative Staph), a type of staph that lives in the nasal passages and thrives in toxic terrain.
If your sinus symptoms keep rebounding, mold exposure should be on your radar.
Bacterial Infections & Biofilms: The Invisibility Cloaks
Chronic sinus infections often aren’t “new” infections at all.
They’re old, unresolved ones hiding in plain sight, shielded by biofilms, sticky webs that bacteria create to evade your immune system and antibiotics (5, 7, 13, 14, 17, 20).
Think of biofilms as invisible fortresses.
Inside, bacteria can share intel, resist treatment, and quietly keep the inflammation simmering (1, 5, 14).
This is why you feel better for a bit on antibiotics, and then the infection “comes back.” It never actually left.
We Can Help
You’re not doomed to live on decongestants and false hope forever. Start with the Mold Toxicity Quiz to begin connecting your symptoms to what might be lurking in your environment.
Take the QuizSuperantigens & Superinfections: Constant Immune Fire Alarms
Certain pathogens like Staphylococcus aureus produce toxins known as superantigens (17, 20).
These bad actors can flip your immune system into overdrive, triggering a massive, uncoordinated response that creates even more inflammation without resolving the threat.
This immune chaos is like trying to put out a fire by screaming at it.
It doesn’t work, and it exhausts your system in the process.
Parasites: The Uninvited Guests Nobody Talks About
Yes, parasites can mess with your sinuses.
No, you don’t need to have been in a jungle to have them.
Parasites are opportunists; they go where the terrain is weak, and sinuses with sluggish drainage are a great hiding spot.
In some cases, systemic parasitic infections (especially protozoa or helminths) can trigger immune suppression or secondary sinus issues (4, 7).
In others, they’re literally nesting up there—gross, but fixable.
If you’re squeamish, don’t Google sinus parasites. Just know that if your gut terrain is off, your sinus terrain probably is, too.
Dysbiosis of the Sinus Microbiome: When the Balance Breaks
You’ve heard of gut dysbiosis—too many bad microbes, not enough good ones.
But your sinuses have their own microbiome, too.
Healthy sinuses are home to a diverse range of microbes that help regulate inflammation, prevent overgrowth, and support mucosal immunity.
Antibiotics, pollutants, chronic inflammation, and mold can all disrupt that balance.
Once the ecosystem tips into chaos, it’s easier for pathogens to overgrow and harder for your body to bounce back (10, 13, 14, 19).
Viral Reactivation: When the “Cold” Never Really Left
Viral infections of the respiratory tract often precede a sinus infection (5, 11, 12, 13, 14, 17, 19).
Additionally, herpes viruses like EBV, CMV, and HSV-1 can go dormant in the body and then reactivate during times of stress, illness, or toxic exposure.
These reactivations can trigger low-grade, chronic inflammation that contributes to ongoing sinus pressure, immune exhaustion, and even pain.
Most ENTs won’t test for viral load, and you don’t need an active cold sore to be experiencing the fallout.
If you’re dealing with fatigue, fog, and sinus pain that seems to ebb and flow with stress, this could be in the mix.
These aren’t fringe theories. These are under-addressed, well-documented drivers of chronic sinus dysfunction and they change the game once you know they’re there.
But hidden root causes don’t exist in a vacuum. Certain lifestyle and structural factors can make your body even more vulnerable. That’s what we’ll cover next.
Factors That Make It Worse (aka the Gasoline on the Fire)
Let’s say you do finally knock down a sinus infection. You get a few weeks—maybe even a couple months—of relief. And then, boom. It’s back. Again.
This is the part that drives people bonkers. And it’s usually where the medical gaslighting starts: “It must be allergies,” or “Maybe you’re just prone to this.”
(Translation: We don’t know, and we’re not looking deeper.)
If we zoom out, there are a handful of compounding factors that don’t cause sinus infections directly, but they absolutely make it easier for them to linger, rebound, or come back stronger.
Let’s break them down.
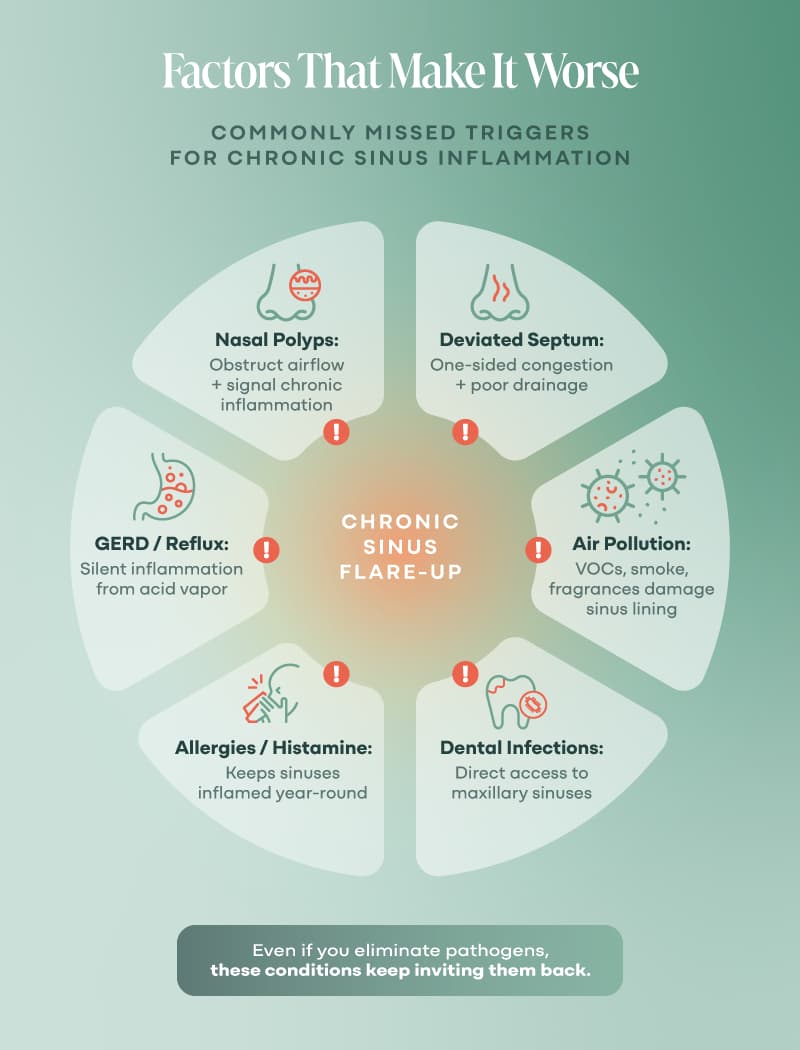
Nasal Polyps
Little benign growths in the nasal passages that can block airflow and drainage (13, 14). They’re often tied to chronic inflammation and mold exposure.
If your sinus pressure feels worse on one side or you’ve lost your sense of smell, this could be in play.
Pro tip: Polyps feed off inflammation. Reduce your toxic load, and you reduce their ability to grow.
Allergies (Environmental + Food)
Histamine overload creates more mucus, more swelling, more congestion.
Even low-level food sensitivities (like gluten or dairy) can keep your tissues inflamed and prone to rebound infections.
Your clue: You feel worse in certain seasons, or after certain meals. But your doctor didn’t connect the dots.
Deviated Septum
If your nasal septum (that thin wall between your nostrils) is off-center, it can restrict airflow and trap mucus (13, 14).
Some people are born with it. Others get it from injury or even bad dental work.
Hint: If one nostril is always more congested, especially at night, this might be your sign.
GERD (Silent Reflux)
Wait, what does acid reflux have to do with sinuses?
A lot, actually.
Stomach acid creeping into your esophagus or throat while you sleep can irritate the upper airway, creating inflammation and making it easier for infections to settle in (8, 13, 14).
Red flag: You wake up congested with a bitter taste in your mouth and throat irritation, especially when lying flat.
Air Pollution & Chemical Exposures
Your sinuses are basically little sponge-lined caves.
If you’re breathing in VOCs, exhaust, synthetic fragrances, or cigarette smoke daily? Those sponges are soaking it all up, causing irritation and inflammation (13, 14, 23)
Environment check: Do you feel better when you leave your house, your job, or your city?
Dental Infections
Your upper molars share a wall with your maxillary sinuses.
That means even a mild root canal infection or abscess can leak bacteria directly into your sinus cavity (13, 14).
Clue: You’ve had dental work on the upper teeth and now deal with sinus pressure on the same side. Coincidence? Probably not.
Individually, these issues may seem minor. But stack them up, and they form a perfect storm, not just for getting sick, but for staying stuck.
And if the deeper terrain isn’t addressed, your body will keep responding the only way it knows how: with inflammation, mucus, and fatigue.
Now that we’ve explored what’s interfering with your healing, let’s talk about why your usual treatments haven’t worked and what’s required to break the cycle.
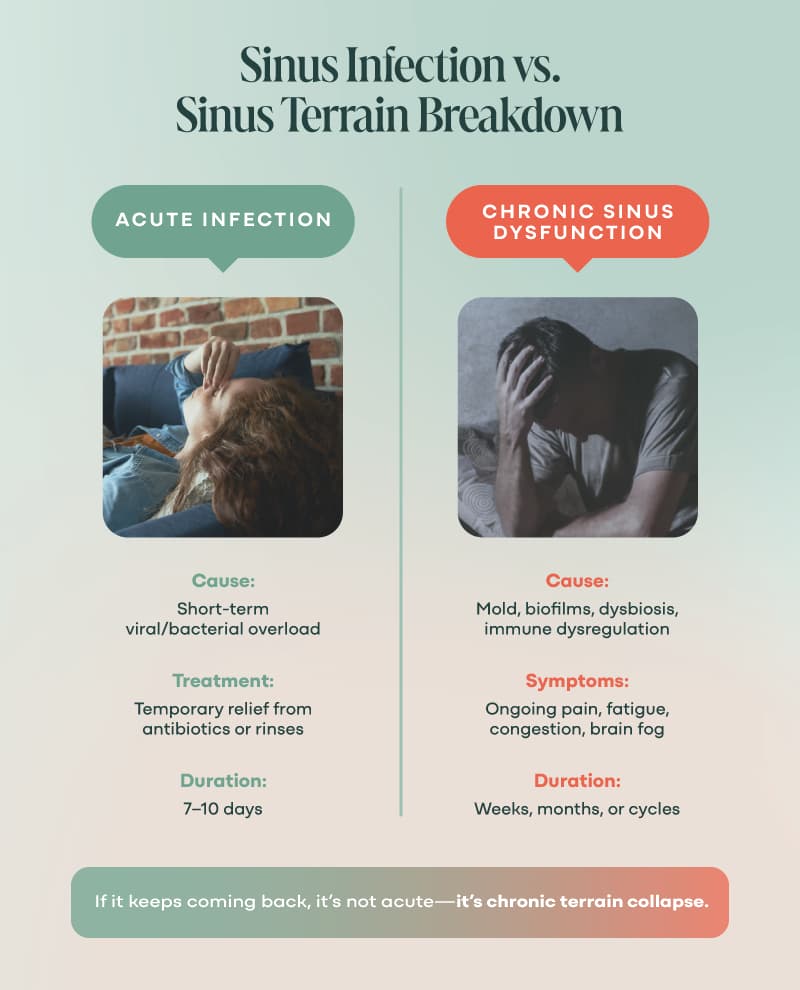
Why This Isn’t Responding to “Standard Treatment”
You’ve probably been prescribed antibiotics for your sinus infections. Maybe multiple times.
And maybe, like a lot of folks, you felt a little better, until it all came roaring back.
Here’s the hard truth: standard sinus treatments are designed for acute infections, not for chronic inflammation, biofilms, or a compromised internal terrain.
And they often miss the real issue entirely.
Chronic sinus issues usually involve biofilm-based colonies, where bacteria have built protective shields to resist both antibiotics and your immune response.
The chronic inflammation induces alterations to the mucosal barrier (5, 10, 13, 17, 18, 19, 21), and mucociliary movement decreases (13, 14, 19).
Mucus builds up, providing nutrition for pathogenic microbes and causing dysbiosis (10, 13, 14, 19). The gut microbiome can even get involved to increase your risk, especially strep, clostridium, oscillospira, and ruminococci (22).
- Antibiotics push an already dysbiotic sinus microbiome further out of balance, and now opportunistic pathogens have even more space to party.
- Nasal corticosteroids reduce swelling and inflammation, but they don’t fix what’s causing it.
- Nasal Rinses help flush debris and allergens, but if your drainage pathways are clogged, your nervous system is dysregulated, or your sinus tissue is inflamed from biofilm or mold, you’re just stirring the pot.
Why You Still Feel Stuck
You’ve been trying to mop up the flood without turning off the faucet.
You’ve been treating symptoms while the root causes keep seeding new infections.
And the more this loop repeats, the more your immune system gets exhausted, and the more chronic everything becomes.
You don’t need another prescription.
You need a new paradigm.
One that understands that terrain is everything and that healing happens when we support the systems your body relies on to detox, drain, and defend.
In the next section, we’ll unpack what your symptoms are really trying to tell you and how to start listening.
Biological Hard-Wiring
By now, it’s probably clear: this isn’t just about your sinuses.
What you’re experiencing is a complex biological feedback loop. And here’s the key shift most people miss: Your symptoms aren’t the enemy. They’re messages pointing you toward what your body is trying to resolve.
The Cell Danger Response
Your body has a built-in alarm system that gets activated when it senses danger, like toxins, infections, or even trauma.
This is called the Cell Danger Response (CDR), a protective state where healing slows down, and the body focuses on survival.
Dr. Robert Naviaux’s research shows that the CDR plays a role in many chronic conditions, including sinus inflammation, by locking your cells in “defense mode.”
In that state (10, 13, 14, 19):
- Mucus production ramps up
- Inflammation becomes chronic
- Drainage pathways shut down
- Energy gets diverted away from repair
Your body’s adapting to ongoing threats it hasn’t been able to clear yet.
Nervous System Dysregulation
Your nervous system is the command center for your healing.
When you’re stuck in sympathetic dominance (fight, flight, freeze, or fawn), your body deprioritizes detox and repair, including the natural flow and drainage of your sinuses.
If your sinuses never fully clear, or every little bug sets you off again, nervous system dysregulation might be the missing piece.
No amount of herbs or antibiotics will work if your body doesn’t feel safe enough to heal.

What You Can Start Doing Differently Right Now
Sinus issues are rooted in deeper imbalances your body’s been begging you to address.
The good news? You don’t have to solve this overnight. You just need to stop putting out fires long enough to rebuild the terrain.
Here’s where to begin.
Calm Your Nervous System—First
If your nervous system doesn’t feel safe, your immune system won’t regulate, your drainage won’t work, and detox becomes just another stressor.
Start with micro-practices:
- Diaphragmatic breathing
- Feet on the earth
- Turning off screens after sundown
- 30 seconds of stillness after brushing your teeth
Regulation doesn’t have to be hard, but it must be consistent.
Follow the Clues
Start by asking better questions:
- What exposures have I had that might still be affecting me (mold, metals, dental work)?
- Do my symptoms ebb and flow with stress, sleep, or diet?
- Have I ever felt fully better, even for a little while?
Your symptoms are data. Track them, don’t fear them.
Suspect Mold? Don’t Guess, Assess
If you’ve lived or worked in a water-damaged building—or if you don’t even know if you have—test.
Mold exposure is the most overlooked cause of persistent sinus inflammation I see.
Take the free mold assessment to start narrowing this down.
Open Your Drainage Pathways
Before you go after infections, you’ve got to open the exits.
Start gently:
- Stay hydrated (yes, this matters more than you think)
- Support your lymph (lymphatic self-massage with “The Big 6,” light movement, castor oil packs)
- Stimulate your Vagus nerve (humming, gargling, splashing cold water on your face, whatever feels doable today)
- Use binders and bitters to support liver and bile flow if you’re ready
Remember: Detox doesn’t just mean you “push it out,” it means you “set the conditions for it to leave.”
Flush for Flow
Once your drainage pathways are open, incorporate a nasal rinse using distilled water and salt. (The Navage is my fave!)
This can remove pathogens and irritants, moisten your sinuses, and remove gummed up mucus (2, 10).
Nasal rinses are one of the low-cost heath tools I can’t live without.

Bringing It All Together
You’ve been told this is “just allergies,” “just aging,” “just stress.”
You’ve been handed nasal sprays, antibiotics, maybe even surgery, and yet here you are. Still congested, still exhausted, still wondering what’s really going on.
The truth is, you’ve probably never had anyone look at your whole story before.
Not your body’s exposures.
Not your nervous system state.
Not your drainage capacity or the deeper terrain.
But we do.
The One Lab Test That Could Change Everything
The Detox Nation Mold Test + Consult is a comprehensive urine test that measures 40 different mycotoxins from 11 mold species—the most complete mold toxicity panel available—plus a 60-minute consultation with our expert team to review your results.
Get Your Mold Test + ConsultIf you’re ready for expert eyes on your case, we can help you map a clear, customized healing strategy that supports your whole body, starting with your sinuses. If you have other health issues like digestive symptoms, chronic fatigue, and inflammation, you may prefer to get personalized support to resolve your health issues.
Apply to work with a Detox Nation practitioner 1:1
This sucks, but it’s fixable.
And you’re not alone.
We’re here to guide you, but you are the CEO of your healing, and you’re in charge of showing up for your own body. It’s totally worth it.
FAQs
Why do my sinus infections keep coming back?
Because the root causes like mold, biofilms, or dysbiosis haven’t been resolved. Killing bacteria isn’t enough when the terrain is still toxic or inflamed.
Could this really be mold?
If you’ve ever lived or worked in a water-damaged building, yes. Mold and mycotoxins are major drivers of chronic sinus issues, and most doctors don’t test for them.
Do I have to do a detox to fix this?
Yes, but not the juice-fast kind. You need a strategic, gentle process to open your drainage pathways and support your body’s natural detox systems.
I don’t feel sick enough for this to be mold or biofilms. Could it still be that?
Yes. Chronic sinus inflammation can smolder quietly for years. You don’t need dramatic symptoms to have serious interference.
How do I know if drainage is blocked?
If your sinuses feel stuck, swollen, or thick (even when you’re not “sick”) that’s a sign your drainage pathways need support.
Do I have to do this alone?
No way. You’re here now, which means you’ve got guidance and community. Healing happens faster when you’re supported.
I don’t have time for this. What if I just keep doing what I’ve been doing?
Chronic sinus infections, when left to their own devices or inadequately treated, can lead to serious neurological complications like meningitis, abscesses, thrombosis, orbital cellulitis, and even epilepsy (13).