Not all menopause symptoms are just hormonal—your mitochondria play a crucial role in energy, brain function, and metabolism. Learn how mitochondrial dysfunction can amplify the signs and symptoms of menopause and what to do about it.
You wake up exhausted.
Your brain feels like it’s stuffed with cotton balls.
Your body aches in places that never used to hurt, and despite eating the same way you always have, the scale seems to be climbing like it has a personal vendetta against you.
You tell yourself it’s probably menopause.
Or aging.
Or maybe you’re just losing your mind.
Your doctor glances at your chart, nods sympathetically, and says something like, “Well, you’re at that stage in life…” and offers either hormones or a prescription for antidepressants.
And yet, deep down, this doesn’t resonate for you.
If this sounds familiar, you might be dealing with mitochondrial dysfunction, not just menopause.
Or both, because life likes to keep things interesting.
Let’s break it down and figure out why you feel like a human-shaped energy crisis.
What Is Menopause? (And Why Does It Feel Like You’re Falling Apart?)
Menopause happens when your ovaries retire and leave you to fend for yourself (11, 14, 25, 29).
Thanks a lot, ovaries!
It’s not their fault – ovaries age faster than other organs (15).
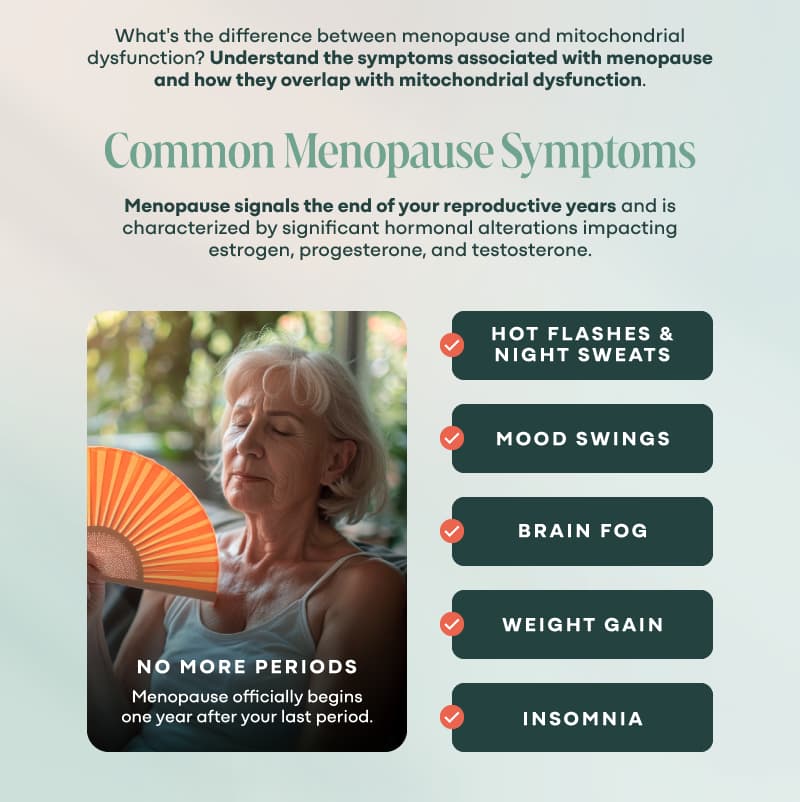
But seriously, menopause signals the end of your reproductive years and is characterized by significant hormonal alterations impacting estrogen, progesterone, and testosterone, as well as thyroid hormones and others (3, 8, 11, 17).
Specifically, estrogen and progesterone plummet, while Follicle Stimulating Hormone levels increase (30).
This results in no more periods (17, 25, 29), but you may be too tired to throw them a farewell party.
DHEA from the adrenal gland becomes your main source of sex hormones, and since its production decreases with age, it can’t keep up (5).
Menopause officially begins one year after your last period, but the chaos leading up to it—perimenopause—can start in your late 30s or early 40s and lasts one year after your last period (7, 29).
During perimenopause, your symptoms can be allll over the place as your hormones are shifting and changing – kind of like puberty in reverse (11).
The “Menopause Transition” can last from one to ten years (23).
Classic Signs and Symptoms of Menopause:
- Hot flashes & night sweats (2, 3, 9, 13, 23, 32, 36) – Why is it 200 degrees in here? Oh wait, it’s just me. This is also called Vasomotor Symptoms of Menopause or VMS.
- Mood swings (8, 9, 13, 17, 18, 19, 23, 29, 30, 32, 34) – One moment you’re fine, the next you’re crying because your doggo looked at you too lovingly.
- Brain fog (3, 9, 34) – Walk into a room, forget why. Open your mouth, forget words.
- Weight gain (9, 17, 18, 24, 29, 32) – Your metabolism suddenly moves at the speed of a DMV employee.
- Insomnia (3, 9, 13, 17, 18, 23, 24, 25, 32, 34, 36) – The universe has decided 3:00 AM is your new meditation hour.
What are some other menopausal symptoms? Glad you asked, because I recently did a DEEEEP dive into the research – check out the FAQs for a comprehensive list!
On average, women experience 7-10 individual symptoms during their menopause transition (3).
Yes, menopause can throw your hormones into upheaval, but it shouldn’t feel like your body is completely breaking down.
If your fatigue, brain fog, or muscle weakness feel extreme, something else may be at play. One possibility is mitochondrial dysfunction.
What Is Mitochondrial Dysfunction? (And Why You Might Feel Like a Dead Phone Battery)
Your mitochondria are the power plants of your cells.
They take the food you eat and the oxygen you breathe and turn them into ATP—your body’s usable energy (38, 53).
When they work well? You feel strong, clear-headed, and full of life.
Not so much? You feel like someone pulled the plug on your entire operating system.
When your mitochondria get damaged, old, and inefficient, they start spitting out more pollution than energy.
Mitochondrial autophagy (or mitophagy) is your body’s natural way to break down and recycle these worn-out mitochondria, so your cells don’t turn into sluggish, toxic wastelands.
Skip this process, and you’re basically running on decades-old, smoke-belching engines instead of sleek, high-efficiency ones.
What Causes Mitochondrial Dysfunction?
While your mitochondria are absolute workhorses, they are vulnerable.
Some of the things that damage mitochondria and cause dysfunction include:
- Deficiencies of key nutrients (54)
- Toxicities from industrial chemicals, processed foods, heavy metals, mold exposure, EMFs, unprocessed emotions, and more (54)
- Damage to the networks that communicate with your mitochondria – think microbiome, neurons, hormones, etc. (Looking at you, parasites!)
- Inflammation
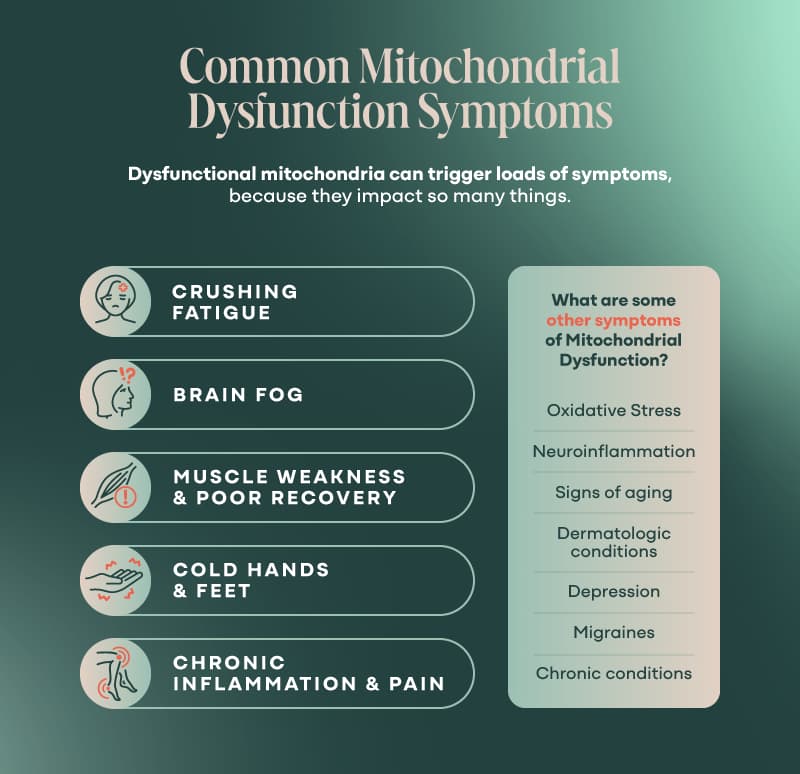
Classic Symptoms of Mitochondrial Dysfunction:
- Crushing fatigue(38) – Not “I need a nap” tired. More like “I could sleep for a week and still feel wrecked.”
- Brain fog (52) – It’s not just forgetfulness; it’s like thinking through molasses.
- Muscle weakness & poor recovery (38) – Your body doesn’t bounce back anymore.
- Cold hands & feet – A sign your cells aren’t producing enough heat.
- Chronic inflammation & pain (52) – Achy joints, tight muscles, random nerve pain.
Sounds a lot like menopause, right?
That’s because mitochondria and hormones are closely linked. When one tanks, the other follows.
For example, estrogen regulates mitochondrial autophagy.
Decreased estrogen impairs your body’s ability to clean out the old or broken mitochondria, resulting in less energy and more oxidative stress (53).
On the other hand, changes in mitochondrial activity can increase ovarian cell aging (43).
What are some other symptoms of Mitochondrial Dysfunction?
- Increased Oxidative Stress and Free Radical Production (44, 50, 52)
- Increased inflammation and neuroinflammation (52)
- Increased neurodegeneration (also Alzheimer’s Disease and Parkinson’s Disease (52)
- Signs of aging (thin skin, hair loss, slow wound healing, dermatitis, etc.) (46)
- Dermatologic conditions such as vitiligo, psoriasis, and lupus (46)
- Depression (41) – But many antidepressant medications inhibit mitochondrial activity (38)
- Migraines (38)
- Chronic conditions such as cardiovascular disease, cancer, metabolic syndrome, and more (40)
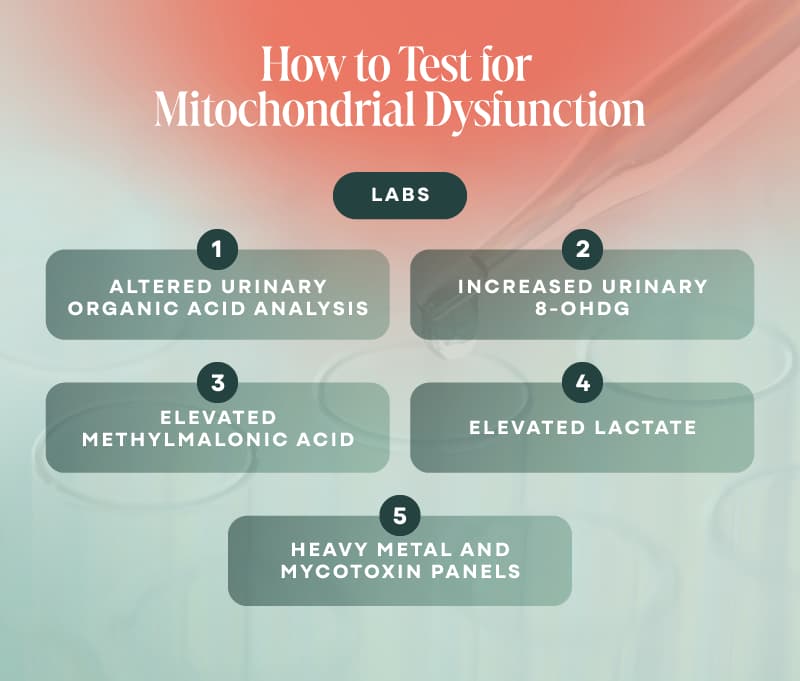
- Labs:
Dysfunctional mitochondria can trigger loads of symptoms, because they impact so many things.
Additionally, your mitochondria are like the “canaries in the coal mine” – they are highly sensitive to stress of all forms and will quickly sound the alarm.
This is called the Cell Danger Response.
The Cell Danger Response
Imagine your cells as tiny, hypervigilant security systems.
When they detect a threat, they slam the panic button and shift into Cell Danger Response (CDR) mode (47, 48, 49, 54).
This means they stop normal functions like energy production, detoxification, and communication with neighboring cells and instead go into full lockdown, hoarding resources to survive (47, 48, 49, 54).
You’re not broken. You just need a recharge.
Whether it’s menopause or mitochondria or both, join our Rapid Energy Reset to give you the information, community, and resources to help you feel like yourself again!
Join Rapid Energy ResetPhases of Cell Danger Response
The Cell Danger Response has three distinct phases. Once initiated, you must complete all three phases to return to normal function.
CDR1: The Alarm Phase (Survival Mode)This is the initial danger detection phase.
Your mitochondria sense a threat—be it an infection, toxin, trauma, radiation, or chronic stress—and go into defense mode (47, 48, 49).
Energy production shifts from ATP (clean fuel) to glycolysis (quick, dirty fuel), inflammation skyrockets, and normal cellular functions like detox, repair, and communication get shut down (47, 48, 49, 54).
Your body feels this as acute fatigue, inflammation, and stress intolerance.
CDR2: The Isolation Phase (Cellular Quarantine)
Now, your body walls off the damaged or infected areas.
Cells become less responsive to outside signals (including hormones and nutrients), tissues stiffen, and chronic inflammation keeps things locked in place.
Just like countries will stop trusting their neighbors and toughen their borders during war, so too do cells when they feel threatened (49).
They will literally create space between themselves and neighboring cells and alter the chemical composition of their cell membranes (48, 50).
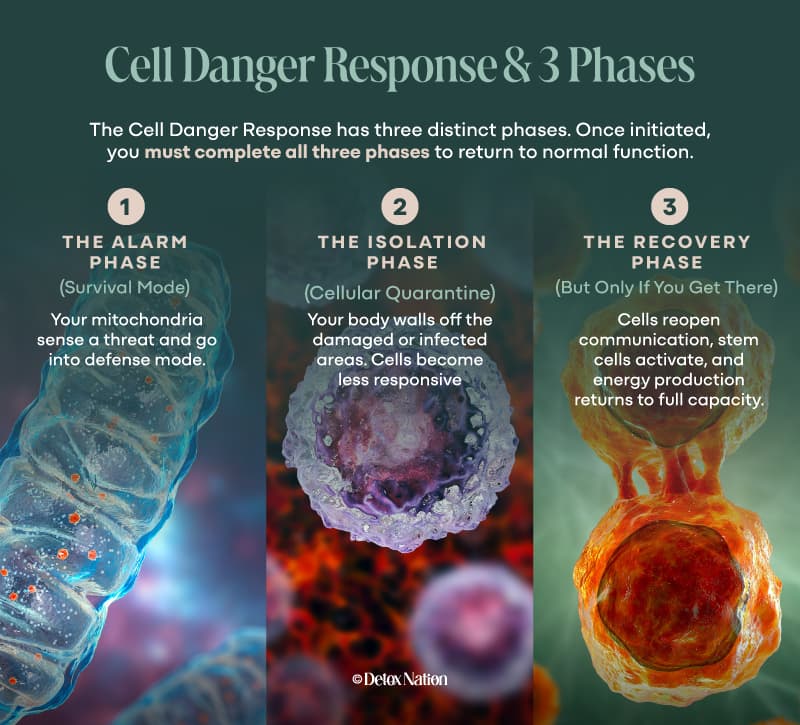
Some cells will generate defense chemicals, while others will sacrifice themselves to save others. In so doing, they release ATP outside of the cells, causing inflammation and perpetuating the CDR (48, 49).
This is where people start feeling long-term fatigue, autoimmunity, or hormone imbalances—because your body won’t fully restore function until the danger is gone.
If you’re dealing with mold, Lyme, heavy metals, or trauma, you’re likely stuck here.
CDR3: The Recovery Phase (But Only If You Get There)
If your body gets the all-clear signal, it rebuilds and resets.
Cells reopen communication, stem cells activate, and energy production returns to full capacity.
But if the original trigger wasn’t fully cleared (or new stressors keep showing up), the body can get stuck between CDR2 and CDR3, leading to lingering issues like chronic illness, brain fog, and metabolic dysfunction.
The big problem?
Most people never fully complete CDR3 because they’re unknowingly re-triggering the alarm—through toxins, infections, unresolved trauma, or just pushing their bodies too hard without adequate recovery.
The key to real healing is figuring out what’s keeping your cells locked in defense mode and giving them the signal that it’s finally safe to recover.
Cell Danger Response and Sympathetic Dominance
When your nervous system gets stuck in sympathetic mode (fight-or-flight), your body is constantly bracing for danger—pumping out stress hormones, shutting down digestion, and keeping you wired but exhausted.
This chronic stress signal feeds right into the CDR, reinforcing the idea that it’s not safe to heal.
Since mitochondria are the first responders in CDR, they interpret all this stress as an ongoing threat, keeping cells in lockdown mode and limiting energy production for anything other than defense.
It’s a vicious cycle: sympathetic dominance fuels CDR, and CDR keeps the body locked in survival mode, making it nearly impossible to shift into parasympathetic (rest and repair) mode.
This is why people stuck in chronic illness often feel like they’re “doing everything right” but not getting better—until the body gets a clear “you’re safe now” signal, true healing stays out of reach.
Cell Danger Response and Menopause
As estrogen declines, so does its protective effect on mitochondria, inflammation, and nervous system regulation.
This makes your cells more prone to perceiving stress as danger, keeping the CDR switch stuck in the “on” position.
Mitochondria—your body’s energy factories and main CDR regulators—become less efficient, leading to fatigue, brain fog, and metabolic slowdowns.
Plus, lower estrogen means higher oxidative stress and reduced autophagy (cellular cleanup), making it even harder to clear out the molecular debris that signals safety to your cells.
On the flip side, if your body was already stuck in CDR before menopause—from chronic infections, toxins, or stress—the transition into menopause can hit even harder.
Since the CDR blocks full healing until the threat is gone, it can amplify menopause symptoms like hot flashes, sleep disturbances, and inflammation, keeping you in a prolonged state of survival mode instead of graceful adaptation.
The key?
Helping your body feel safe enough to step out of CDR, support mitochondrial function, and navigate menopause as a transition—not a battle.
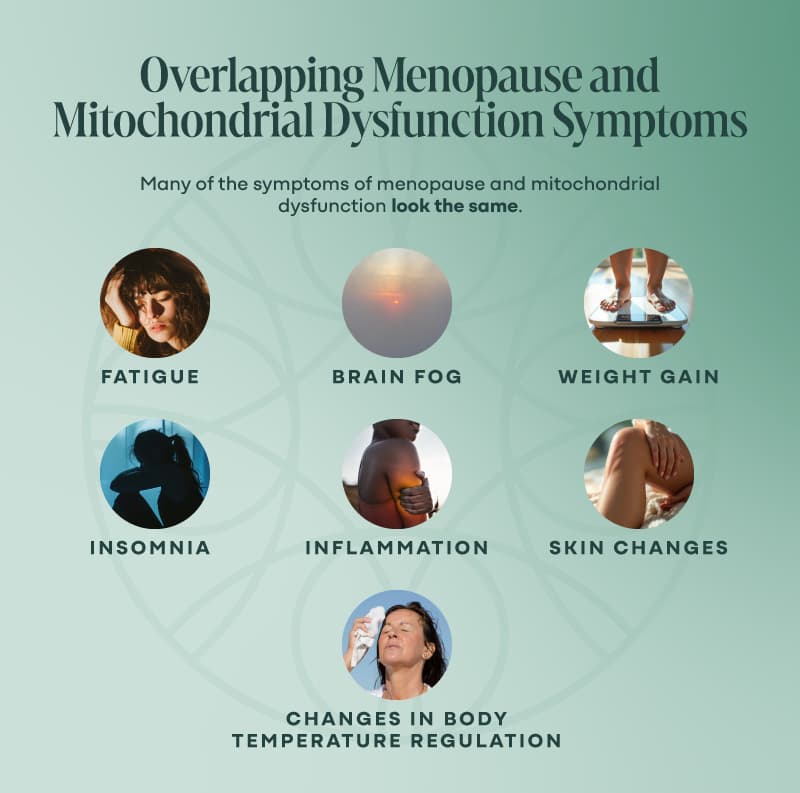
Where Do Menopause and Mitochondrial Dysfunction Overlap?
Here’s the fun part: many of the symptoms of menopause and mitochondrial dysfunction look the same.
- Fatigue – Either your hormones or your mitochondria (or both) are dragging you down.
- Brain fog – Can’t focus? Can’t find words? Welcome to the fog zone.
- Weight gain – Your metabolism isn’t just hormonal—it’s cellular energy, too.
- Insomnia – Low estrogen, adrenal dysfunction, or mitochondrial shutdown can all disrupt sleep.
- Changes in Body Temperature Regulation – Can be either or both, lucky you!
- Inflammation – So many things cause inflammation – foods, pollution, toxins, chemicals, metals, mold, EMFs, parasites, and the list goes on.
- Skin Changes – Found with aging, mitochondrial dysfunction, and hormonal shifts.
So how do you know which one is the culprit?
Key Differences: Is It Menopause or Mitochondria?
Here’s an example of ways to think about different symptoms to get a better idea if they’re due to menopause or mitochondria.
- Sudden vs. Gradual Decline
- If your symptoms came on suddenly with skipped periods, hot flashes, and mood swings, think Menopause.
-
- If your decline has been slow and relentless for years, think Mitochondria.
- Exercise Recovery
- If even a short workout leaves you exhausted for days, it’s mitochondrial dysfunction.
- If you just feel sluggish but bounce back quickly, it’s more likely hormonal.
- Sensitivity to Smells, Chemicals, or Toxins
- If perfumes, alcohol, or even cleaning products didn’t bother you before, but now make you feel awful, that’s a mitochondrial red flag.
- Temperature Regulation
- Menopause: Hot flashes, night sweats, overheating.
- Mitochondria: Cold hands/feet, can’t warm up, wildly fluctuating body temperature.
- How You Feel After Eating
- Mitochondria issue: You feel wiped out after meals, especially carbs.
- Hormonal issue: Blood sugar dips make you hangry or anxious.
- Brain Fog
- Menopausal brain fog is inconsistent—it comes and goes with hormonal fluctuations.
- Mitochondrial brain fog is relentless. Thinking feels like wading through mud every single day.
As we can see, there’s a lot of overlap between symptoms of menopause and mitochondrial dysfunction.
Sometimes you can spot the difference, sometimes you can’t, and sometimes it really is BOTH.
What do you DO about it?
The Good News: How to Support Both Naturally
Step 1: Mitochondria-Friendly Nutrition & Detox
- Ditch the sugar & processed foods – Nothing slows mitochondria down like ultra-processed junk.
- Eat more protein & healthy fats – Fuel for both hormones and cellular energy.
- Mitochondrial support supplements: Make sure to talk to your practitioner to determine specifically what YOUR body needs and to obtain reputable brands.
- CoQ10 (energy production)
- PQQ (mitochondrial repair)
- Magnesium (critical for energy & hormones)
- B vitamins (for ATP production)
Step 2: Drainage and Detox Pathways Matter
Your mitochondria can’t thrive in a toxic body. Support drainage and detox with:
- Infrared sauna (sweating out toxins = happier mitochondria)
- Binders like activated charcoal (help remove heavy metals & mycotoxins)
- Lymphatic movement (rebounding, dry brushing)
Step 3: Lifestyle Upgrades That Help Both
- Morning sunlight – Regulates circadian rhythms & boosts mitochondria.
- Strength training – Muscle = more mitochondria = more energy.
- Cold exposure & breathwork – Resets the nervous system and improves cellular function.
Step 4: Emotional Stress & Trauma Healing
- Mitochondria store trauma. Chronic stress keeps them in survival mode.
- Somatic work, nervous system regulation, and trauma release can unlock energy.
Closing Thoughts: You’re Not Alone (And You Deserve Answers)
If you’ve been dismissed with “it’s just aging” and handed a prescription, you’re not alone.
Your symptoms are real.
Menopause and mitochondrial dysfunction are deeply connected. Addressing both means:
- More energy
- Better brain function
- Hormones that cooperate
FAQ: Quick Answers to Your Biggest Questions
Q1. Can you have mitochondrial dysfunction without menopause symptoms?
Yes! Mitochondrial dysfunction can happen at any age due to toxins, stress, or poor diet.
Q2. Will hormone therapy fix mitochondrial dysfunction?
Not necessarily—if your mitochondria are struggling, addressing energy production and detox pathways is key.
Q3.I don’t have hot flashes—could it still be menopause?
Yes. Not all women experience symptoms such as hot flashes during menopause. Some experience:
- Brain fog
- Fatigue
- Weight gain
- Mood swings
If these symptoms fluctuate over time, it’s more likely hormonal. If they’re constantly getting worse, it’s time to check your mitochondria.
Q4. Can stress affect both menopause and mitochondria?
Yes! Chronic stress wipes out mitochondria and makes menopause symptoms worse.
- Stress increases cortisol, which burns through magnesium & B vitamins (critical for mitochondria).
- High stress = more oxidative damage, which ages mitochondria faster.
- Poor stress resilience can make menopausal symptoms unbearable.
Supporting stress recovery (breathwork, magnesium, adaptogens) can help both mitochondria and hormones.
Q5. I feel cold all the time—what does that mean?
Cold hands, cold feet, or feeling chilled when others are warm = mitochondrial dysfunction.
Mitochondria create body heat as they produce energy. If they’re struggling, you’ll run cold no matter how many sweaters you put on.
Q6. How long does it take to improve mitochondrial function?
It depends on how long they’ve been struggling.
- Some people feel dramatic improvement in a few weeks with diet & lifestyle changes.
- Others take a few months to fully rebuild energy production.
The key? Remove mitochondrial stressors (toxins, processed foods, chronic stress) and nourish your cells.
Q7. Can menopause and mitochondrial dysfunction be misdiagnosed as other conditions?
Yes! Both conditions mimic:
- Chronic fatigue syndrome (low mitochondrial function)
- Fibromyalgia (inflammation + energy depletion)
- Hypothyroidism (sluggish metabolism)
- Depression/anxiety (mitochondria affect neurotransmitters)
If you’ve been diagnosed with one of these, but treatments aren’t helping, consider checking mitochondrial health.
Q8. What’re the biggest red flags that mitochondria are the problem?
Your symptoms don’t fluctuate with your menstrual cycle.
You feel worse after exercise instead of better.
You feel cold, weak, or chemically sensitive.
If your body feels like it’s running on empty, no matter what you do, your mitochondria need help.
You’re not broken. You just need a recharge.
Whether it’s menopause or mitochondria or both, join our Rapid Energy Reset to give you the information, community, and resources to help you feel like yourself again!
Join Rapid Energy ResetQ9. Can you provide a comprehensive list of symptoms associated with menopause?
Yes – here they are – holy smokes there are a TON! Every woman may experience symptoms of menopause differently. Some may have mild symptoms; others may have symptoms for several years leading up to menopause. Menopause may cause:
- Genitourinary Syndrome of Menopause (GSM) are experienced by up to half of all menopausal women (29). These symptoms include vaginal dryness, vulvovaginal irritation, genital pain with sex, itching, urinary urgency, urinary incontinence, pain with urination, bacterial vaginosis, UTIs, tissue fragility, vaginal dysbiosis, and more (5, 6, 24, 30, 33, 34, 37). There may be physical changes to the lower urinary tract, vagina, and vulva, such as atrophy, pale color, dryness, and bleeding (4, 9).
- Hypoactive Sexual Desire Disorder (HSDD): This is emotional distress due to a continued loss of sexual desire or interest. There’s some overlap here, as painful sex, decreased lubrication, and decreased orgasm of GSM contribute to HSDD (6, 18, 31).
- Vasomotor Symptoms of Menopause (VMS) are reported by almost 80% of women (17, 18, 29). This includes the notorious night sweats and hot flashes (2, 3, 9, 13, 23, 32, 36). Did you know that roughly 10% of women can have hot flashes and night sweats for more than 10-15 years following menopause (2, 17)? Yikes!
- Musculoskeletal Syndrome of Menopause (MSM) is found in over 70% of menopausal women (34). This includes: decreased muscle mass (sarcopenia), joint pain, loss of strength, decreased bone density, increased osteoarthritis, increased risk of fracture, and increased risk of tendon or ligament injury (3, 13, 24, 34). Low back pain is also common (18).
- Sleep Disturbances: Trouble falling asleep, trouble staying asleep, waking up early, and increased sleepiness during waking hours are found in menopause (3, 9, 13, 17, 18, 23, 24, 25, 32, 34, 36).
- Neurological, Cognitive, and Emotional Changes:
- Changes to circadian rhythm (25).
- Neurotransmitter fluctuations (8, 19)
- Depression (reported by almost 40% of menopausal women) (29, 30).
- Memory problems or brain fog (3, 9, 34)
- Difficulty concentrating (9)
- Mood changes (anxiety, depression, etc.) (8, 9, 13, 17, 18, 19, 23, 29, 30, 32, 34)
- Headaches (3, 9, 18)
- Vertigo (9)
- Tinnitus (9)
- Decreased cognitive function (3, 17, 18, 19)
- Brain changes
- Sympathetic Dominance (27)
- Low Brain Derived Neurotrophic Factor (44)
- Increased risk of Alzheimer’s Disease (44, 53)
- Digestive Disturbances:
- Metabolic Changes:
- Cardiovascular Changes:
- Accumulation of fat around the waistline and heart (9, 10, 24, 26, 29)
- Changes to the physical structure of the heart and heart function (29)
- Elevated risk of diabetes, cardiovascular disease, insulin resistance (2, 3, 13, 28, 29, 30, 32, 53)
- Dyslipidemia (32, 35)
- Palpitations (3, 9)
- Increased blood pressure (32)
The good news?
You won’t experience all these symptoms, and the symptoms you DO experience can be resolved.
Q10. What diseases can be connected to Cell Danger Response?
Autism spectrum disorders, ADHD, asthma, food and chemical sensitivities, emphysema, Tourette’s, mental health disorders (such as bipolar disorder, schizophrenia, and post-traumatic stress disorder), chronic traumatic encephalopathy (CTE), traumatic brain injury (TBI), epilepsy, diabetes, kidney, liver, and heart disease, cancer, neurodegenerative diseases (such as Alzheimer’s and Parkinson’s), and autoimmune disorders (such as lupus, rheumatoid arthritis, and multiple sclerosis). (47)