Chronic sinus symptoms and sinusitis can wreak havoc in your life. Unlike bacterial and viral sinusitis, fungal sinusitis – including allergic fungal sinusitis – can be difficult to resolve. But you can heal your fungal sinus infection!
So, you’re stuffed up again, huh?
You know that feeling when your sinuses are clogged, your head feels like it’s underwater, and no amount of nose-blowing brings relief?
You’ve tried all the decongestants, been through rounds of antibiotics, and still can’t shake that sinus pressure, congestion, and overall yucky feeling.
I hate to break it to you, but there’s a sneaky culprit that could be the real reason your sinuses feel like a construction zone — mold.
Yeah, mold. That gross stuff in your bathroom tiles, your air vents, or, heaven forbid, your favorite old book collection.
You might be thinking, “Okay, I get seasonal allergies, but mold in my sinuses? Really?”
Yes, really.
Fungal sinusitis is a special kind of torture.
It’s not your typical viral or bacterial infection — it’s a stubborn, often hidden fungal invasion that can hijack your respiratory system, your energy, and your memory.
But don’t panic. While it does suck, it’s fixable.
Let’s look at what fungal sinusitis really is, how you can tell if mold is playing hide-and-seek in your sinuses, and what you can do to evict this unwelcome guest for good.
Key Takeaways
- Chronic sinus symptoms may be caused by mold.
- Mold can hide in multiple places in your environment.
- You can resolve chronic fungal sinusitis
What is Fungal Sinusitis?
Fungal sinusitis is an infection caused by fungi in your nasal passages. No, really? Let’s be more specific!
Types of Fungal Sinusitis and Causes
Fungal sinusitis comes in various forms, but there are two broad categories: Non-invasive (the most common) and invasive.
Invasive Fungal Sinusitis is a rare type of fungal infection and is typically found in the immunocompromised.
In these cases, the fungi penetrate the tissues and is extremely difficult to address (28). Luckily, this is not the type of fungal sinusitis I want to talk to you about!
Noninvasive fungal sinusitis is generally less severe but can affect seemingly healthy people. Subcategories include:
- Fungal ball where clumps of fungus grow in the sinuses. (I know it’s totally different, but this always makes me think of a hair ball in cats!)
- Saprophytic fungal sinusitis – This is where mold grows on crusted mucus or dead tissue but doesn’t actually infect the nasal tissue itself. Totally gross, but this is the least of the sinus-mold evils.
- Allergic fungal sinusitis happens when your body reacts to the fungus like an allergen. (As such, it’s classified as a type of Allergic Airway Disease (10).) It also has subcategories (because of course it does!):
- Chronic Rhinosinusitis (CRS) – with or without nasal polyps
- Allergic Fungal Rhinosinusitis (AFRS)
- Allergic Bronchopulmonary Aspergillosis (ABPA)
Chronic Rhinosinusitis is an inflammation of the mucosal tissue lining your nose and sinuses.
In a 2014 study, 41 species of mold in 12 genera were detected in an astonishing sixty-seven percent of samples taken from participants with CRS (6). The most common molds detected were Penicillium spp. and Aspergillus spp.
In a case study of a family who had been diagnosed with CRS, penicillium and aspergillus were cultured, and mycotoxins were found in stool, urine, nasal secretions, and breast milk (8). (Even the family doggo had mold and mycotoxin issues!)
Allergic Fungal Rhinosinusitis is characterized by increased eosinophils (a type of white blood cell), fungal hyphae in the mucus, enlarged sinuses, hypersensitivity to fungal pieces, and an exaggerated Type 2 immune response (2). This abnormal immune response actually helps the fungi stick around (10, 11, 12).
Yes, you read that right. The mold triggers an immune response, but instead of the normal immune response, which eliminates the infection, it’s an abnormal response that benefits the mold. Sneaky little buggers!
Allergic Fungal Rhinosinusitis (AFRS) and Allergic Bronchopulmonary Aspergillosis (ABPA) are thought to be essentially the same thing, just in different parts of the respiratory system (9).
In a study of people with AFRS and ABPA, mold was cultured from the nasal secretions of ninety-seven percent of the participants (9). Which mold, you ask? Aspergillus. (Shocking, I know.)
Further, mold was found in almost 50% of air samples taken from the participants homes. Again, asss…pergillus.
To keep it simple, I’m going to refer to the Allergic Fungal Rhinosinusitis “family” as Fungal Sinusitis in this article!
You got this!
To get started, take my quick Mold Assessment Quiz to see if mold might be the cause of your fungal sinusitis!
Take The Mold Assessment Now!How is it Fungal Sinusitis Different from Bacterial or Viral Sinusitis?
In fungal sinusitis, tiny fungi (mold) cause the issue instead of bacteria or viruses.
Bacterial and viral sinus infections typically resolve relatively quickly with antibiotics or antiviral medications.
In contrast, fungal sinusitis can be harder to address even with antifungal medications or surgery.
Spoiler alert: The best way to resolve moldy sinuses is with a comprehensive holistic approach that addresses root causes and supports your immune system.
Risk Factors
Certain factors can increase your likelihood of getting fungal sinusitis.
A weakened immune system, from conditions like diabetes or ongoing steroid use, raises risk levels.
Other immune system destroyers include:
- Eating the Standard American Diet of ultra-processed industrial food products (it’s no coincidence that the acronym for this is SAD.)
- Poor sleep (Scrolling through social media at 2am?)
- High stress
- Hormonal imbalances
- Exposures to industrial chemicals and toxins
- A sedentary lifestyle
- Opportunistic infections with freeloading parasites
- EMF exposure
- Mycotoxin exposure
- Certain prescription medications
- Digestive issues like Leaky Gut
Basically, being an average American harms your immune system!
Frequent exposure to mold or living in warm, damp areas can also contribute. Mold loves humid locations, so your sinuses are a perfect home for them!
Common Fungal Sinusitis Symptoms
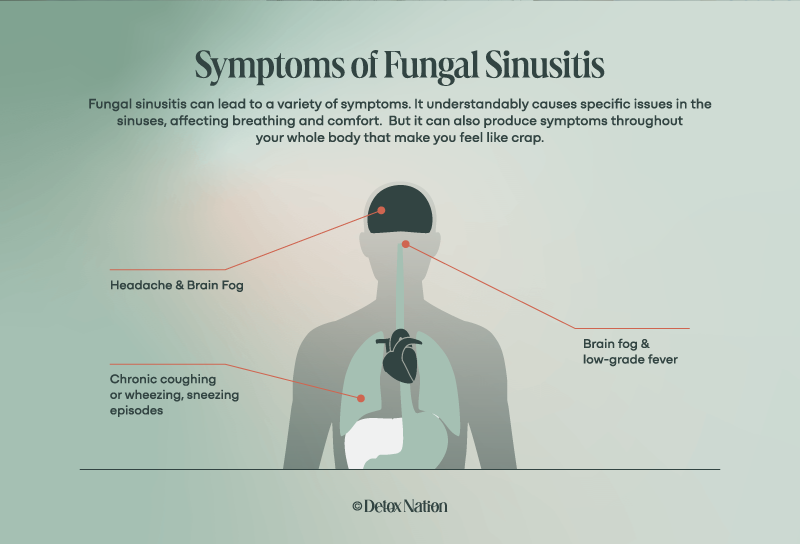
Fungal sinusitis can lead to a variety of symptoms. It understandably causes specific issues in the sinuses, affecting breathing and comfort. But it can also produce symptoms throughout your whole body that make you feel like crap.
Sinus-Specific Symptoms
Anything growing in your sinuses that doesn’t belong there can be pretty uncomfortable.
You may have sinus pain, which feels like a dull, throbbing ache around the eyes, nose, or forehead. (It can “hurt so good” to press on these spots, but you can’t have your fingers on your face all day!)
You might notice a constant post-nasal drip or thick nasal mucus that makes you swallow more frequently. The mucus running into your stomach can make you feel full or even nauseous. (An all-mucus diet? No thank you!)
Nasal congestion and a runny nose are annoying and make it hard to breathe easily.
The pressure can build up in your face, especially around your forehead and eyes, leading to headaches or a heavy feeling.
You might lose your sense of smell or taste, making your food flavorless and your meals boring.
Sound fun yet? There’s more!
Systemic Symptoms
Besides affecting your sinuses, fungal sinusitis can make you feel yucky in general.
You may develop a low-grade fever, a sign that your body is reacting to a foreign invader.
You can also feel bone-weary fatigue that is out of synch with your activities. For example, you make a quick grocery run but then collapse into bed for three hours.
Your focus and memory can decrease as you experience “brain fog,” making it hard to concentrate at work or school. Some examples of brain fog are:
- Walking into a room then forgetting why you’re there
- Forgetting a person’s name or part of a conversation within minutes
- Reading a book, but your mind keeps wandering. No matter how hard you try to focus, you find yourself rereading the same sentence.
Sound familiar?
You might have chronic coughing or wheezing due to the constant irritation of the mold (21,22).
Sneezing episodes that are like a full-on sneeze symphony can leave you breathless.
These symptoms can significantly affect your day-to-day life, making simple tasks feel more challenging.

How Does Mold Cause Sinus Problems?
Mold is a known trigger for sinus issues, leading to discomfort and health concerns. When mold spores are present in the environment, they can be inhaled, causing inflammation in sensitive areas like the sinuses.
The Mold Connection
Mold spores are everywhere and can easily enter your body with every breath.
They thrive in damp and warm places, both indoors and outdoors. And in your body!
I should mention that the most common indoor mold species are none other than our “friends” Aspergillus and Penicillium.
When you inhale these spores, they enter your sinus cavities.
Within 24-hours, then can embed, or colonize, in your sinuses and start pumping out their nasty mycotoxins.
By the way, the chances of mold colonization in your sinuses increase in the presence of bacteria (26). Like the bacteria we have living all over and inside our bodies? Yup, just like that.
Once inside your sinuses, mold produces a protective “invisibility cloak” called “biofilm” that makes it harder for your body to detect them (26).
It also makes it hard for any treatment you may try to reach them.
Mold – hijacking and hiding your sinuses – can stay and generate toxins long after your initial exposure (27).
Put Your Thinking Cap On
Unfortunately, there’s not a ton of research on the mechanisms and impact of chronic mold colonization in your sinuses. (Most of the research focuses on the invasive-type of infection, or on medications for the non-invasive type.)
This is where we have to blend common sense with the information we DO have.
Let’s look at an area that has more research: Mold, mycotoxins, and the gut.
- Mold and mycotoxins, whether they enter your body by touching, eating, or inhaling, suppress your immune system (20).
- This causes systemic and local inflammation (18, 20).
- Mucus production by the gut lining decreases (13).
- An imbalance between the “good” and “bad” gut bacteria occurs (17, 19).
- Stomach acid and bile production decrease, impairing your digestion (15, 16).
- All of this leads to damaged connections between the cells that line your gut (epithelial cells), and they can’t protect you anymore (13). Waste materials and toxins are allowed to re-enter your bloodstream instead of being eliminated. This is called “Leaky Gut Syndrome.”
We know that the airways have a microbiome and are also lined with mucus-producing cells.
Likewise, I believe that mold and mycotoxins can suppress your immune system, cause systemic and local inflammation, decrease mucus production, alter the airway microbiome, and damage the connections between the cells that line your airway.
Here’s some support from the literature:
- Environmental fungi (like the mold causing the musty smell in your home or office) are being recognized as having a causal role in airway mycosis (10).
- CRS is marked by immune system dysregulation and dysfunctional airway epithelium (11).
- Type 2 immune responses increase sinus inflammation and decrease airway microbiome diversity (3)
- “AFRS is characterized by defects in the mucosal barrier and permissive sinus environment for fungal germination.” (10)
- Gut microflora changes contribute to the chronicity of sinusitis (5).
- Inflammatory airway diseases have been found to be associated with “building-related intolerances” [read: mold] and “chemical intolerances.” (7)
We may not have this all wrapped up in one study, but we can connect the dots between studies!

Could Mold in Your Home Be the Source?
Mold in your home can be a big concern, especially when it leads to health issues like fungal sinusitis.
Common Sources of Mold Exposure
Environmental mold exposure is related to symptoms and illness (1, 7, 8, 9). So absolutely your home or office could be causing your fungal sinusitis!
Mold tends to grow in damp places in your like your bathrooms, kitchen, and basement, and it thrives on materials like wet wood, old books, or even the clothes in your closets.
Leaks in roofs, windows, or pipes are common sources, as are HVAC systems.
Tell-Tale Signs of Mold
Often, mold is hidden, but visible signs can include spots or discoloration on walls and ceilings.
That peeling wallpaper that you’ve been avoiding? Yeah, it might have mold growing under it.
You might notice a musty smell, which is another indicator of mold presence.
Symptoms that only seem to happen when you’re at certain places like your damp basement or that old office building could hint at mold exposure.

Limitations of Conventional Treatments
Conventional treatments, while sometimes helpful, have limitations.
Medications usually treat symptoms and don’t always address the root causes, leading to potential relapses in persistent fungal environments.
Surgery, despite being a more direct approach, doesn’t ensure long-term success and can be fraught with complications.
Resolving chronic rhinosinusitis requires more than just tackling the current infection.
You need to maintain a healthy living environment to reduce the chances of re-infection after treatment.
You also need to address the internal factors that made your body a good host for mold.
Root Cause Treatment
Resolving fungal sinusitis requires targeting the root causes.
Environmental Detox
Removing sources of mold from your surroundings is essential. Here are some tips!
- Start with mold remediation to eliminate any existing mold.
- Decrease humidity to below 50% using dehumidifiers and increase ventilation by opening windows or using fans.
- Throw out contaminated items like carpets or wallpaper that can’t be cleaned.
- Find and fix leaks immediately.
- Clean small mold patches with vinegar or hydrogen peroxide. Do not try to clean large areas by yourself – contact a professional mold remediation company.
- Digitize important papers, documents, and photos so they don’t make you sick.
- Donate clothes you no longer wear so mold can’t snack on them.
- Always wear protective gear when cleaning mold to avoid exposure.
Detox Your Body
Cleansing your body supports healing.
Consider Epsom salt baths or dry brushing to help your body get rid of toxins. (Yes! You have many good reasons to relax in a warm bath!
Drink plenty of distilled water to keep your body hydrated and flush out impurities.
Support immune function by eating a balanced diet and taking supplements if needed.
Prioritize restful sleep and minimize stress to maintain a strong immune response.
Minimize exposure to EMF’s, industrial chemicals, and seed-oils.
Consult with a mold-literate practitioner to provide personalized detox strategies tailored to your needs.
Conclusion
Dealing with fungal sinusitis is like having a moldy roommate living in your nose rent-free — super annoying and harmful in the long run.
The good news? You don’t have to tolerate it.
By addressing both your external environment (hello, moldy bathroom corners) and the internal conditions that allow mold to settle in your body, you can reclaim your health and breathe easier.
To get started, take my quick Mold Assessment Quiz to see if mold might be the cause of your fungal sinusitis!
It’s time to kick mold to the curb for good. This isn’t something that just “goes away” with antibiotics or surgery — you need to dig deeper, both literally and figuratively. Roll up your sleeves, detox your house, and give your body the support it needs to kick fungus out.
You got this!
To get started, take my quick Mold Assessment Quiz to see if mold might be the cause of your fungal sinusitis!
Take The Mold Assessment Now!Frequently Asked Questions
Fungal sinusitis includes a range of symptoms, treatment options, and potential risks.
How can someone tell if they have a fungal sinus infection?
Identifying a fungal sinus infection often involves the following symptoms: nasal congestion, facial pain, and headaches. Sometimes, there’s a decreased sense of smell.
What can be done to treat a fungal infection in the sinuses?
Treatment usually depends on the type and severity of the infection. Common approaches include antifungal medications prescribed by your healthcare provider or even sinus surgery. A Root Cause Approach is the best way to resolve CFS.
Can nasal sprays help clear up fungal infections in the sinuses?
Nasal sprays may aid in managing symptoms of chronic rhinosinusitis but aren’t a standalone solution for fungal infections. They can help reduce inflammation and relieve sinus pressure and congestion. However, antifungal treatments are usually needed alongside nasal sprays to tackle the actual infection.
Does fungal sinusitis have a distinct odor?
Yes, it can sometimes produce a unique smell. This can happen due to the presence of fungi in the sinuses. If you notice a strange persistent odor, it might be worth checking with a healthcare professional for further evaluation.